Intractable dry eye caused by dysfunction of meibomian gland treated with IPL
Serap Yurttaser Ocak . Sezen Karakus. Osman Bulut Ocak, et. Int Ophthalmol. 2020. 01(08)
Objective: To investigate the effect of intense pulsed light (IPL) on meibomian gland dysfunction (MGD) and dry eyes.
Methods: The follow-up records of patients with MGD treated by IPL were studied retrospectively. Dry eye assessment was conducted by means of the ocular surface disease index (OSDI) score, the frequency of using artificial tears, tear film rupture time (NIBUT), meibomian gland atrophy score, corneal staining score and Schirmer test. The data of patients at the initial stage of the first admission treatment, and at the time of 1 month, 3 months and 12 months of follow-up were analyzed. According to the severity of their baseline meibomian gland abscission score, they were divided into mild Moderate and severe atrophy.
Results: The results from 43 cases (22 cases of mild atrophy, 17 cases of moderate atrophy, and 4 cases of severe atrophy) showed that, except for the Schirmer test, all dry eye parameters of mild and moderate atrophy patients after treatment were significantly improved, and this effect lasted until the 12 month follow-up period (p<0.001). At any follow-up time point, there was no significant improvement in any parameters of patients with severe meibomian atrophy (p>0.05). In mild and moderate atrophy groups, OSDI score and NIBUT began to improve at 1 month (p<0.01), while corneal staining and meibomian gland abscission score began to improve at 3 months at the earliest (p<0.01). No adverse reaction was observed except 4 patients with temporary skin redness and swelling.
Conclusion: IPL is a safe and effective treatment for MGD patients. This study shows that IPL can improve the early symptoms and signs of MGD, and has a beneficial effect on the long-term treatment of patients with meibomian atrophy.
正Analy
Meibomian gland dysfunction (MGD) is a common disease, with a prevalence rate of 5-20% in western countries and 45-70% in Asian populations. MGD is a chronic diffuse meibomian gland anomaly, usually characterized by obstruction of terminal ducts and changes in gland secretion. These characteristics can directly lead to tear film changes, irritation symptoms, inflammatory reactions and ocular surface diseases. If not treated early, it will lead to inevitable permanent gland damage.
In this article, the authors studied the effects of IPL treatment on the structure of meibomian gland and dry eye symptoms in MGD patients.
Between April and June 2017, 43 patients with initial diagnosis of MGD agreed to receive LLLT-IPL treatment. The average age of patients was 56 ± 12.2 years old. The proportion of female patients was higher (86%), and the proportion of female patients to male patients was 6:1. There were 22 cases of mild atrophy, 17 cases of moderate atrophy and 4 cases of severe atrophy.
There was no significant difference in age or sex between the two groups. In terms of dry eye measurement, there was no significant difference between mild atrophy group and moderate atrophy group (p>0.05), while all dry eye measurements in severe atrophy group were significantly worse. The treatment results are as follows:
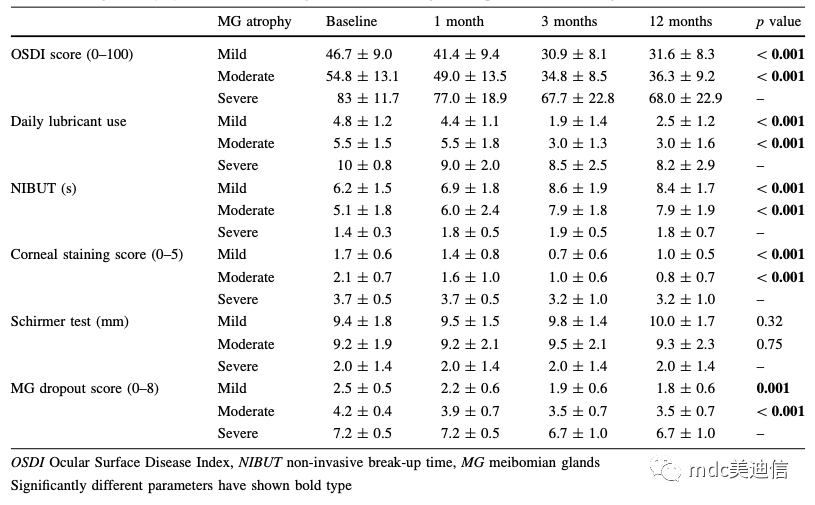
Table 1 Changes of dry eye indicators for evaluation of meibomian gland atrophy according to follow-up time
In the study group of mild and moderate patients, the effect of treatment on the reported symptoms of patients measured with the OSDI questionnaire was evaluated. Over time, the OSDI scores of mild and moderate atrophy groups improved significantly (p<0.001, both are applicable) (as shown in Table 1).
The comparison between mild and moderate atrophy groups showed that the severity of symptoms began to improve significantly at the earliest one month, and could continue to be followed up for three months. Although there was no further improvement after 3 months of follow-up (p>0.05), the OSDI scores of mild and moderate atrophy groups remained stable before 12 months of follow-up (p=0.37 and 0.42 respectively) (as shown in Figure A below).
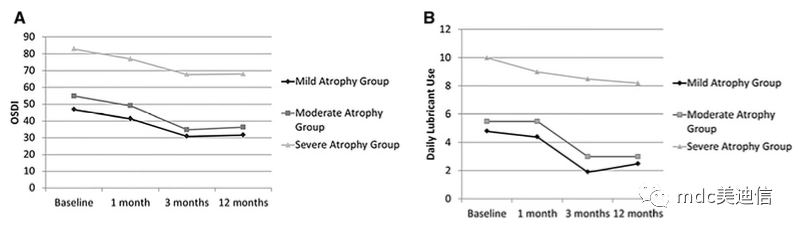
As time went on, the frequency of using artificial tears every day in patients with mild to moderate meibomian atrophy decreased significantly (p<0.001). Before the 3-month follow-up visit, the incidence rate of mild and moderate atrophy groups did not decrease significantly (both p<0.001), and no further changes were found after this time point (as shown in Figure B above).
Over time, NIBUT and corneal staining scores of patients with mild to moderate meibomian atrophy improved significantly (both p<0.001) (Table 1). The follow-up of NIBUT showed that, except for the difference between the 3-month and 12-month mean values, the difference between each group of mild and moderate atrophy groups was significant. This shows that the treatment effect improved continuously from 1 month (p=0.001 and 0.006) to 3 months (1 month and 3 months respectively in the two groups, p<0.001), and continued to 12 months of follow-up (3 months and 12 months, p>0.99, the efficacy of the two groups remained stable). (As shown in Figure A below)
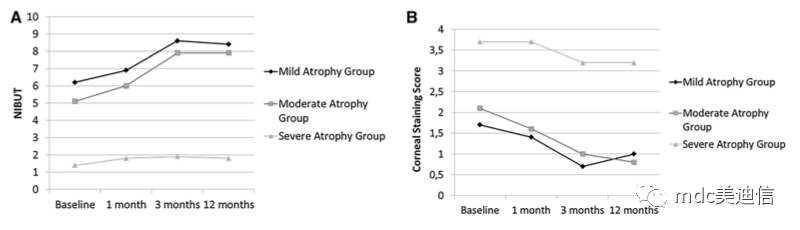
The comparison between groups of corneal staining scores at different time points showed that the mild atrophy group was significantly improved at the 3-month follow-up (p<0.001), but there was no significant improvement before the follow-up and at the 12 month follow-up (p=0.34 and 0.09) (as shown in Figure B above). In the moderate atrophy group, the treatment effect was observed from 1 month (p=0.01), continued to increase until the 3-month follow-up (p<0.001), and remained stable during the 12-month follow-up (p=0.98) (as shown in Figure B above).
No improvement (p>0.05) was found in any study group at any time point in the detection of Schirmer test (as shown in Table 1 and Figure C below).
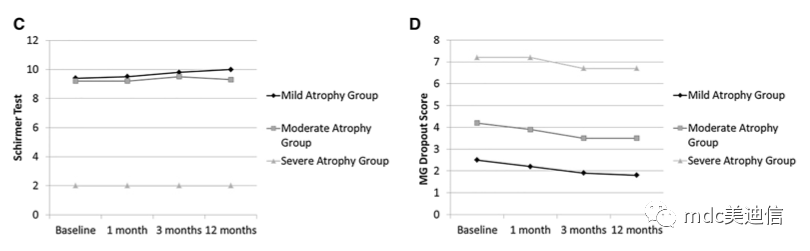
Over time, the meibomian gland scores of patients with mild to moderate meibomian atrophy improved significantly (p=0.001 and<0.001) (Table 1). The follow-up comparison between the two groups showed that it was significantly improved in the three-month observation (p=0.001 and<0.001), but there was no difference in the previous detection (p>0.05 for the two groups). The treatment effect remained stable before the 12-month follow-up (p>0.05 for the two groups) (as shown in Figure D above)
During the 12 months of follow-up in 43 patients, the meibomian atrophy score of 29 patients (67%) decreased by at least 1 point. The scores of the remaining 14 patients (33%) did not change (but did not deteriorate) after treatment. When grouped according to the study, the meibomian atrophy scores of 15 cases (51%) in the mild atrophy group, 12 cases (41%) in the moderate atrophy group, and 2 cases (50%) in the severe atrophy group were improved.
In this study, we explored that IPL is a safe and effective treatment option for patients with MGD. The mechanism of IPL treatment is still unclear. In other literatures, it is pointed out that the possible mechanisms of IPL include:
a. Abnormal vascularization, reducing inflammatory mediators of eyelid and meibomian gland;
b. Heating and liquefaction of meibomian gland secretion;
c. Reduce the metabolism of epithelial cells;
d. Photoregulation;
e. Activating fibroblasts;
f. Regulate the secretion of proinflammatory and anti-inflammatory factors;
Karaca et al. hypothesized that the possible therapeutic mechanism of IPL is nervous system. They believed that the flash of the lower eyelid and temporal part could stimulate the two branches of the parasympathetic nerve, which would restore normal activity of the meibomian gland.
Another important result of this study is that the effect of IPL can last for a long time. During follow-up, it was found that the improvement of physical signs and clinical symptoms could last for 1 year, and no patient's condition deteriorated. In our study, it has been shown that the long-term effect of this new therapy may be due to permanent cell changes in the meibomian gland. This hypothesis can be supported by the following facts: the improvement of the structure of the meibomian gland will last for 1 year, and the score of meibomian atrophy will also continue to decline.

